A new randomized clinical trial has found that targeted therapy for the less impaired arm in stroke survivors can lead to significant improvements in movement and control. The study, conducted by researchers from Penn State and the University of Southern California (USC), was published on February 2 in JAMA Neurology.
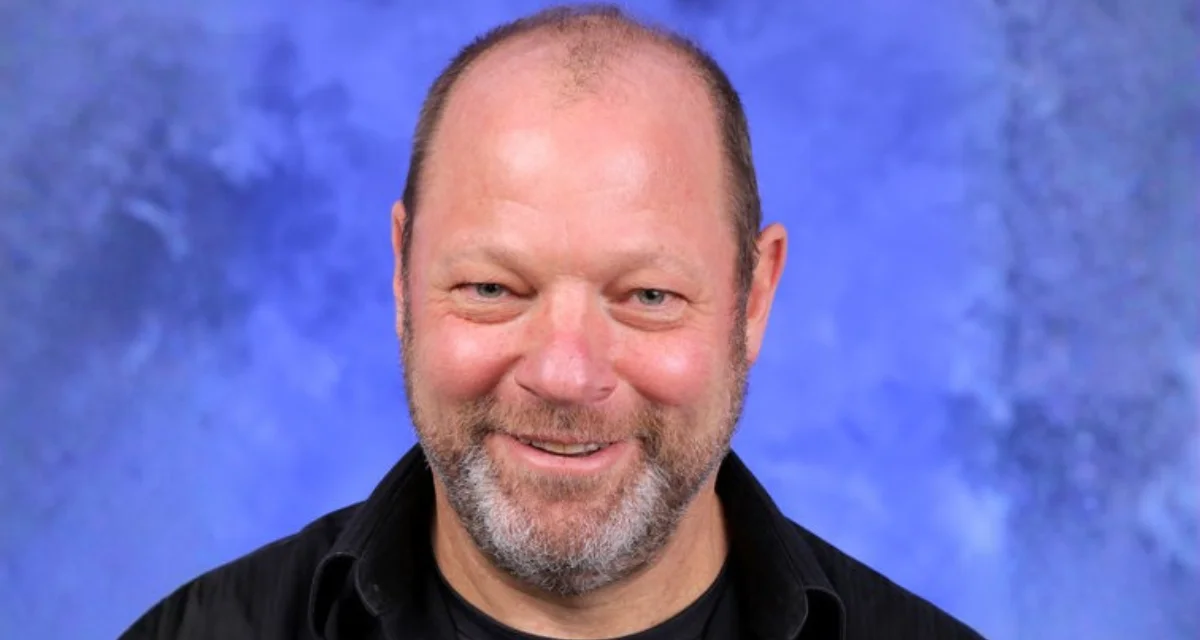
Traditionally, stroke rehabilitation focuses on restoring function to the more impaired side of the body. However, according to Robert Sainburg, co-author of the study and Dorothy F. and J. Lloyd Huck Distinguished Chair in Kinesiology and Neurology at Penn State, this approach overlooks deficits that often exist in the less-impaired arm. Sainburg explained that even when one arm appears normal after a stroke, it may still lose a considerable amount of function, which can be challenging for patients who rely on that arm for daily tasks.
"You're already doing things mostly with one hand and that's really hard in itself," Sainburg said. "Now, the effect of the stroke on the less-impaired arm has added an additional deficit on top of that, say a 10-to-25% loss of motor coordination in the hand that has the most function. That's a big deal in terms of what tasks you can perform for yourself and what tasks require assistance."
The research team noted that while there is extensive research into improving performance in the more impaired or "bad" arm after a stroke, there are few evidence-based interventions targeting the so-called "good" arm. Carolee Winstein, professor emerita and adjunct faculty at USC's biokinesiology and physical therapy department and co-principal investigator of the study, said: "This is the first project to use a rigorous randomized clinical trial design to investigate the use of ipsilesional limb training - training the less-impaired arm - in chronic stroke survivors with severe paresis."
The phase II clinical trial included 53 participants who had experienced a stroke at least three months prior—some many years earlier—and had severe impairment in one arm. Participants were randomly assigned to either receive targeted therapy for their less-impaired arm or standard best-practice therapy for their more-impaired arm over five weeks.
The targeted therapy group engaged in dexterity training using real-world activities as well as virtual reality games designed to address specific deficits based on which side of their brain was affected by stroke. The control group received traditional therapy focused on stretching, therapeutic exercises, and task-specific practice with their more-impaired arm.
At the end of five weeks, those who received targeted training for their less-impaired arms showed notable improvement compared to those receiving standard care. They completed dexterity tests—including picking up small objects and simulated feeding—12% faster than before treatment.
"Stroke patients might have been able to do things like fasten a button, but it took so much time to do it that it wasn't worth it to do it independently. By getting a little bit faster, it makes them want to try to do it by themselves," said Maenza, another author involved with the study. "This can be life changing not just for the patient but also for their spouse or caregiver because the burden of care is reduced."
These gains persisted for at least six months following therapy completion. Sainburg attributed this durability to what therapists call a virtuous cycle: "The targeted intervention puts patients on what therapists call a virtuous cycle," he said. "Once you get a little bit of function, you use it and things continue to improve."
The researchers plan further studies combining this approach with other rehabilitation methods aimed at supporting everyday function.
"Our results open the door to further research directions such as multi-modal approaches where you combine ipsilesional limb training, as was done here, with training that targets both arms, where each side is controlled in unique ways by the nervous system," Winstein said.
Other contributors include Terrence Murphy (Penn State), Nick Kitchen (Penn State), Jennifer Tanaka (USC), Jisung Yuk (Case Western Reserve University School of Medicine), and Rini Varghese (Johns Hopkins School of Medicine). The work was funded by grants from the National Institutes of Health's Eunice Kennedy Shriver National Institute of Child Health and Human Development.