Researchers at the University of California San Diego School of Medicine have conducted what they describe as the first clinical trial to show that cancer drug treatments can be tailored to the unique DNA profile of a patient's tumor. The findings, published in the Journal of Clinical Oncology on January 8, 2026, indicate that using molecular testing to individualize multi-drug treatments based on specific tumor mutations can improve treatment outcomes.
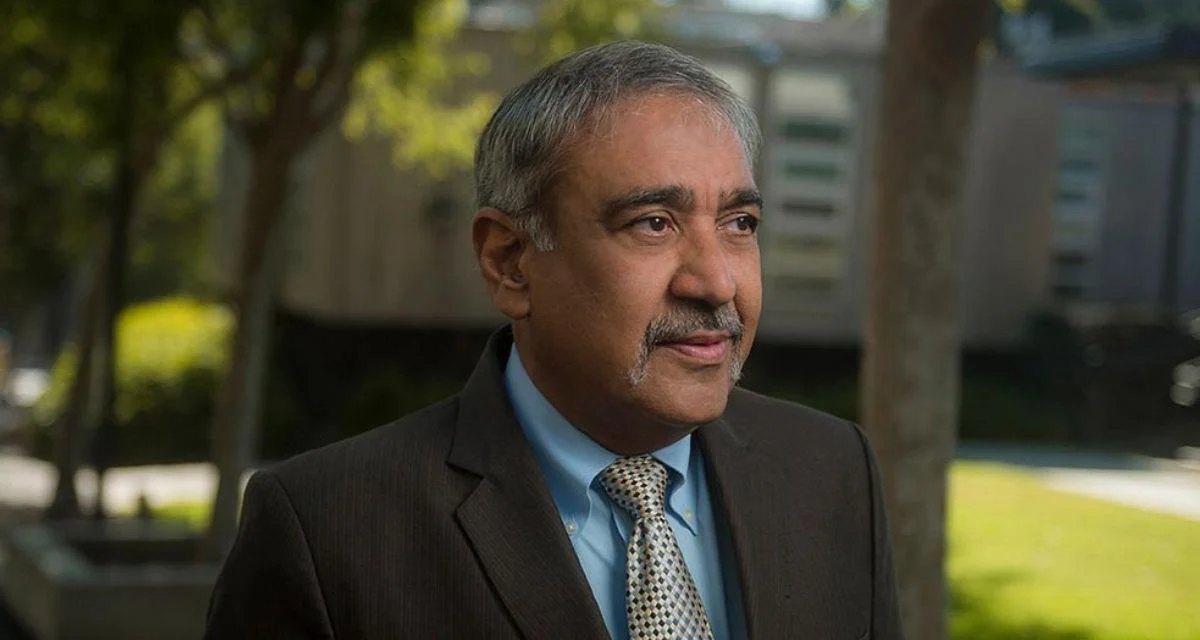
"Every patient and every cancer is unique, and so should how we treat for them," said Jason Sicklick, MD, senior author of the study, professor of surgery and pharmacology at UC San Diego School of Medicine and surgical oncologist at UC San Diego Health. "Our findings demonstrate that precision oncology at the individual level is achievable. When every patient's treatment is guided by their tumor's distinctive DNA, we can treat cancer with better accuracy."
The trial, called Investigation of Profile-Related Evidence Determining Individualized Cancer Therapy (I-PREDICT), used genomic sequencing to identify genetic changes in each patient's cancer. Clinicians then created personalized treatment plans using FDA-approved drugs and adjusted doses to target those specific alterations.
In a group of 210 patients with advanced cancers, almost all had different tumor DNA profiles. This led to 157 separate treatment regimens and included 103 new drug pairings not previously tested together. Patients whose therapies were most closely matched to their tumor mutations saw better responses and improved survival rates. The study found that these new drug combinations did not cause more severe side effects compared to standard treatments.
Starting new drug combinations at lower doses and increasing them gradually helped maintain safety even when combining therapies for the first time.
"The I-PREDICT study shows what's possible when we let a patient's biology guide their treatment," said Shumei Kato, MD, associate professor of medicine at UC San Diego School of Medicine and medical oncologist at UC San Diego Health. "By using biomarkers to select drugs and adjust doses, we can design combinations that precisely target the drivers of each person's cancer."
Diane Simeone, MD, director of Moores Cancer Center at UC San Diego Health added: "Innovative clinical trial design is a central part of what we do at Moores Cancer Center. This study reflects the strength of our multi-disciplinary team-based approach, combining scientific leadership, clinical trial expertise and the infrastructure needed to bring discoveries directly to patients. It's a powerful example of how we're shaping the future of precision oncology and placing the patient at the center of every decision."
Sicklick and Kato are both members of UC San Diego Moores Cancer Center which played a key role in supporting this clinical trial.
Moores Cancer Center is recognized as the only National Cancer Institute-designated Comprehensive Cancer Center in its region and has been ranked among America's top 50 centers for cancer care by U.S. News & World Report.
Sicklick emphasized that this research represents a shift in cancer care strategy: "Instead of a one-size-fits-all, we're moving toward one-size-fits-one," he said.
This research builds on earlier studies published in Nature Medicine (2019) and Genome Medicine (2022) involving subsets from the I-PREDICT cohort but now includes more patients with longer follow-up periods. The latest publication also provides detailed guidance for other organizations interested in adopting similar approaches.
Plans are underway for a randomized trial designed to further confirm these results regarding personalized precision oncology methods.
Additional contributors include Daisuke Nishizaki, Hirotaka Miyashita, Ryosuke Okamura, Michael E. Hahn, Mina Nikanjam, Paul T. Fanta, David E. Piccioni, Hitendra Patel, Ramez N. Eskander, Rana R. McKay, Jeffrey S. Ross, J. Jack Lee, Scott M. Lippman, Shumei Kato and Razelle Kurzrock from UC San Diego.
Funding was provided by Foundation Medicine; Joan and Irwin Jacobs Foundation; Jon Strong; and grants from the National Institutes of Health (P30 CA023100).