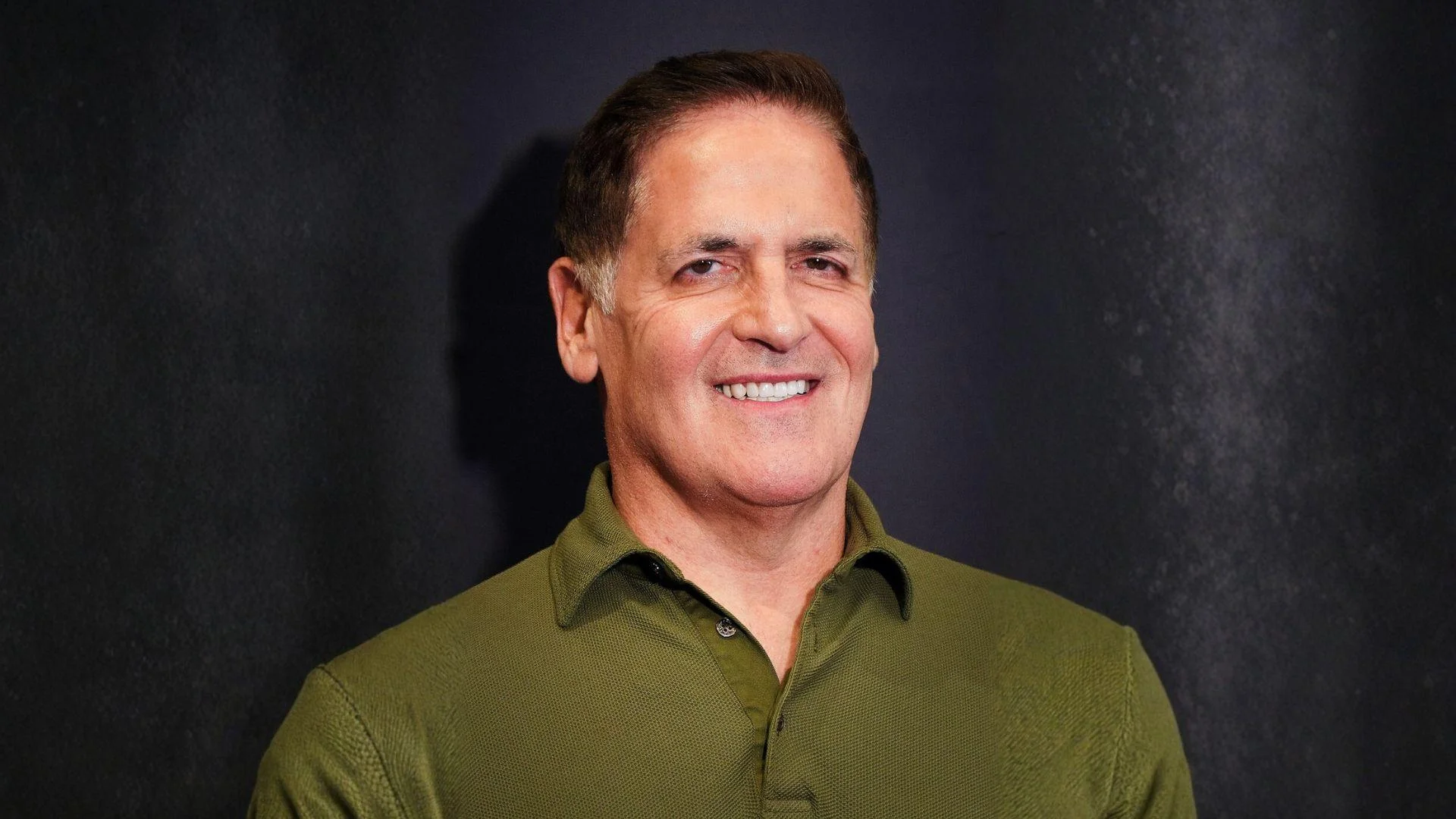
Mark Cuban, an American businessman and founder of the Mark Cuban Cost Plus Drug Company, said that pharmacy benefit managers (PBMs) increase costs by obscuring margins and manipulating pricing, despite their claims of offering the best prices.
"It's like—what's the movie, The Usual Suspects, where they said the greatest lie the devil ever told was telling you they don't exist? The greatest lie ever told by PBMs is that they get the best price for you," said Cuban. "PBMs are owned by the biggest insurance companies. And they play that game of where to hide the margin and how to manipulate pricing, all day, every day."
Pharmacy benefit managers play a central role in managing prescription drug benefits for approximately 270 million Americans. They control which drugs are covered and at what price through complex rebate and fee structures. According to a 2025 Federal Trade Commission (FTC) report, the six largest PBMs collectively process about 90% of all prescription claims in the United States, granting them significant influence over drug pricing and pharmacy networks.
The FTC's second interim staff report on PBMs found substantial price markups by the "Big 3" PBMs—Caremark (CVS), Express Scripts (Cigna), and Optum Rx (UnitedHealth)—on specialty generics, including cancer and HIV drugs. The report described how vertically integrated PBMs can inflate costs and disadvantage independent pharmacies, undermining affordability for patients.
A House Oversight Committee 2024 report revealed that large PBMs use rebates and formulary positioning to secure preferred tiers for higher-priced drugs. This practice makes it more challenging for lower-cost competitors—including generics and biosimilars—to gain access. Evidence showed that PBMs regularly placed costlier options more favorably, a practice that can increase overall spending for employers, insurers, and patients.
PBM practices have also drawn scrutiny in the 340B program, where payers reduce reimbursement or add fees when a claim is flagged as 340B, diverting savings from covered entities. In response, states are adopting "anti-discrimination" laws to curb PBM tactics such as lower payment rates, network exclusion, and contract terms aimed at 340B claims; Nevada's protections took effect on January 1, 2024, joining a growing list of states.
Cuban co-founded Cost Plus Drugs with a model that posts transparent prices calculated as acquisition cost plus a 15% markup, along with a pharmacy service fee and shipping. The model aims to bypass PBM middlemen and pass savings directly to consumers. The company details its pricing method and fees publicly in its FAQ section, emphasizing transparency to counter opaque PBM practices linked to higher drug costs.