Mike Crapo, chairman of the U.S. Senate Finance Committee, announced that the new bipartisan PBM Price Transparency and Accountability Act aims to enhance transparency in pharmacy benefit manager (PBM) operations, safeguard pharmacy access, and reduce prescription costs for patients and taxpayers. This information was released in a statement on the committee’s website.
"Pharmacy benefit managers should not profit from overcharging patients for their prescriptions," said Crapo. "This bipartisan legislation is a decisive step toward making the prescription drug market easier to navigate for both patients and pharmacies. These proposals form a strong foundation for additional efforts to promote pharmacy access, demystify drug pricing and reduce costs for both taxpayers and seniors."
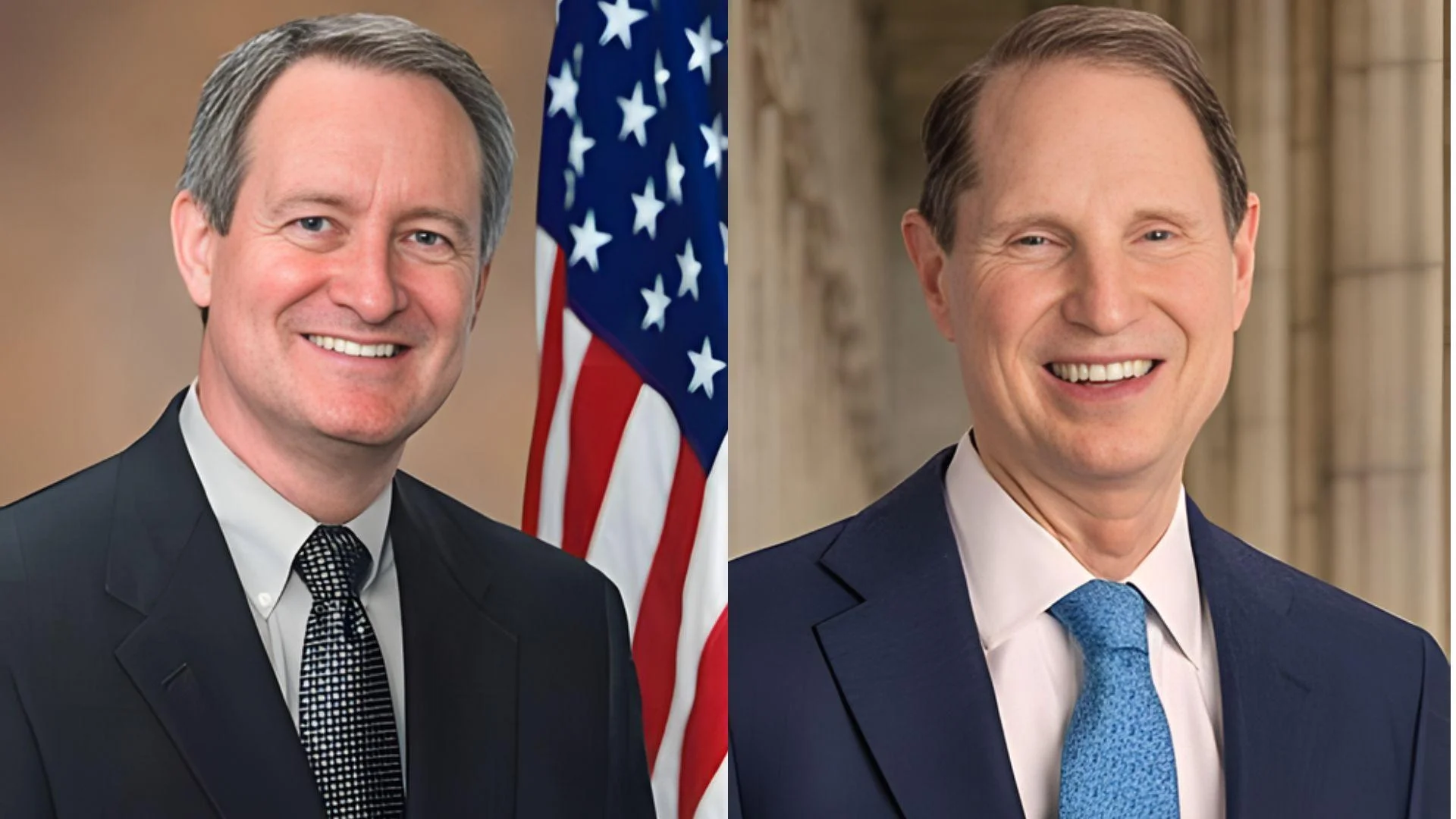
On December 4, 2025, Finance Committee leaders Mike Crapo (R-Idaho) and Ron Wyden (D-Oregon) introduced the bipartisan PBM Price Transparency and Accountability Act. The legislation seeks to separate PBM compensation from rebates, increase reporting and audits in Medicare Part D, protect "any willing pharmacy," require broader participation in the National Average Drug Acquisition Cost (NADAC), and ensure Medicaid payments are made directly to pharmacies. The bill has garnered support from 19 bipartisan co-sponsors.
According to an interim report by the Federal Trade Commission (FTC), there is significant concentration within the PBM industry. The three largest PBMs—OptumRx, CVS Caremark, and Express Scripts—manage approximately 79% of U.S. prescription claims, with the top six controlling over 90%. The FTC warned that vertical integration and opaque rebate practices could inflate drug costs and disadvantage independent pharmacies, prompting calls for reform and increased transparency.
The scrutiny of PBM practices extends to the 340B program, where payers reportedly reduce reimbursement or add fees when a claim is flagged as 340B, diverting savings from covered entities. In response to these practices, states are enacting "anti-discrimination" laws aimed at curbing tactics such as lower payment rates, network exclusion, and contract terms targeting 340B claims; Nevada’s protections took effect on January 1, 2024.
Crapo has been a member of the Senate Finance Committee since 2005 and assumed the role of Chairman in January 2025 after serving as the panel’s top Republican from 2021 to 2025. He has represented Idaho in the U.S. Senate since 1999 and currently leads the committee responsible for overseeing tax, trade, health, and Social Security policy—placing him at the forefront of federal drug-pricing oversight.