The U.S. Vice Presidential debate held earlier this week U.S. Sen. J.D. Vance (R-Ohio) and Gov. Tim Walz (D-Minn.) touched upon rising health care costs, but failed to mention one of fastest-growing federal health programs in existence: The federal 340b drug program.
Established in 1992, the 340b program is facilitated by the Health Resources and Services Administration (HRSA) and enables eligible hospitals and healthcare organizations to purchase outpatient medications at significantly discounted prices. Hospitals participating in the program can use the savings to fund essential services and programs, such as free or low-cost medication assistance, expanded access to healthcare, and community outreach initiatives.
Participating hospitals, however, “often extend their 340B discounts to clinics in well-off communities, where they can charge privately insured patients more than those on Medicaid,” reported the Wall Street Journal.
“In some cases, the program appears to be bolstering profits in well-off areas more than it is underwriting services in less-privileged neighborhoods,” said the Journal article.
Spending on prescription drugs purchased at participating health care providers through the federal 340b drug discount program increased 19% annually between 2010 and 2021, according to a Congressional Budget Office (CBO) report released June 17.
“Eighty-eight percent of the growth in 340B spending from 2010 to 2021 can be attributed to spending on drugs prescribed by hospitals and their affiliated off-site clinics,” said a presentation on the report provided by Rebecca Sachs and Joshua Varcie of the CBO’s Health Analysis Division.
Amidst this rapid growth, Naomi Lopez, senior fellow at The Goldwater Institute, told Show-Me State Times earlier this year that “we don’t actually know” if drug discounts are being passed to patients by organizations participating in the 340b program.
“The real problem is that we don't know if they're making a huge profit, where those profits are going, or if those funds are actually going to care for the low income indigent population,” said Lopez. “We're definitely looking at billions of dollars, and we don't actually know because of the lack of transparency and accountability in the program.”
Due to these transparency concerns, one of the world’s largest pharmaceutical manufacturers — Johnson & Johnson — last month made a novel proposal to ensure drug savings are making their way to patients: Provide rebates instead of discounts to hospitals serving low-income communities.
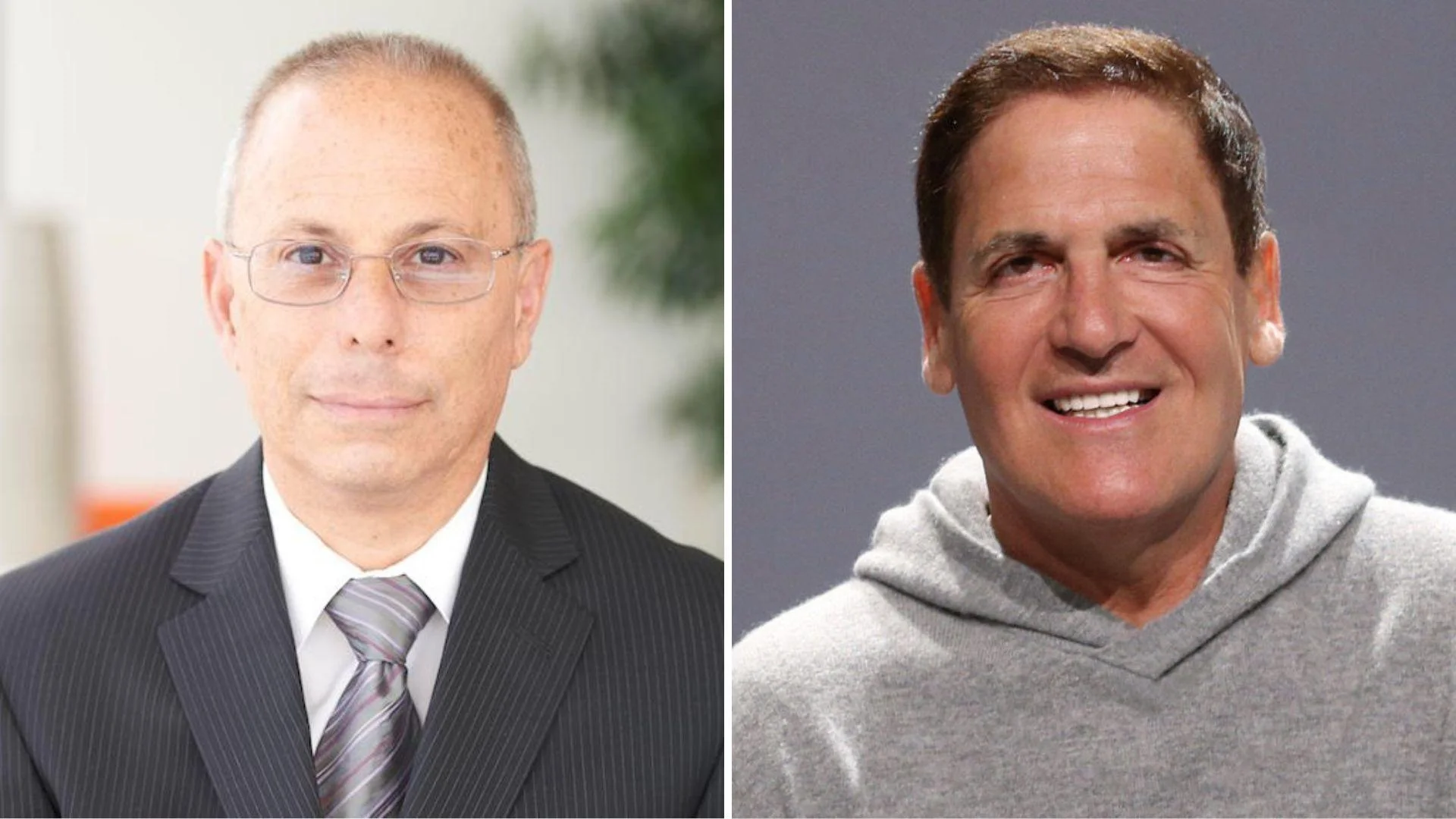
“On August 23rd, Johnson & Johnson announced that disproportionate share hospitals serving low-income patients will receive 340B discounts on Xarelto and Stelara through rebates, rather than upfront discounts,” wrote Peter Pitts, former FDA Associate Commissioner, in a Sept. 12 RealClearHealth op-ed. “Under this new arrangement, hospitals will receive 340B prices only after submitting certain medical, purchase and dispensing data.
“In other words, ‘trust, but verify,’” wrote Pitts.
While Johnson & Johnson faced pushback from hospitals, some legislators, and HRSA, the company’s proposal found a sympathetic ear in billionaire “Shark Tank” entrepreneur Mark Cuban, founder of Cost Plus Drugs.
“I think this is to reduce the significant amount of fraud that Johnson & Johnson (and other manufacturers face),” Cuban posted on X. “Every single meeting I have had with a drug manufacturer has included a discussion about 340b fraud amounting to tens of millions of dollars or more.”
“It looks like Johnson & Johnson is just asking to be able to fully audit claims in a reasonable period of time,” said Cuban. “Do you see anything in this program that would prevent eligible patients or hospitals from getting the discount they are entitled to? I haven’t so far.”
Pitts, in his RealClearHealth op-ed, wrote that hospitals “hate transparency” because “they’re hiding some very dirty laundry.”
“A February 2024 PatientRightsAdvocate.org report found that just 689 (34.5%) of 2,000 hospitals it examined were fully compliant with federal price transparency rules,” Pitts wrote. “That’s down from 721 (36%) that were found to be fully compliant from the organization's last report, from July 2023.”
“Per the new report, the most common reason for noncompliance was missing or significantly incomplete pricing data,” he wrote. “And it’s getting worse -- the analysis found that 135 hospitals that were previously compliant are now noncompliant.”
There have been several proposals in Congress to address transparency concerns with the 340b program.
U.S. Sen. John Kennedy (R-La.) introduced a bill in 2023 that he said would ensure “that organizations are transparent about how they use resources from” 340B.
Earlier this year, U.S. Reps. Larry Bucshon, MD (R-IN-08), Buddy Carter (R-GA-01), and Diana Harshbarger (R-TN-01) introduced the introduced the "340B Affording Care for Communities and Ensuring a Strong Safety-Net Act" to increase oversight and transparency in the 340B drug pricing program.
Neither of these proposals has advanced on Capitol Hill.
Whether or not the Johnson & Johnson rebate proposal becomes a reality, it has put the fast-growing 340b program in the spotlight with a new approach that may end up shaping the legislative and regulatory approach that determines the future of the program.