Tennessee, like other states, is dealing with health-care insurance-provider plans to scale back participation in its Affordable Care Act Marketplace exchange in 2017, but monopolies are not being created in counties where only one provider will remain, an industry expert said.
"Monopoly" is not the correct word, Nate Purpura, director of public relations and communications for eHealth, Inc, the nation's largest private online marketplace for health insurance, said during a Patient Daily interview.
"When you use that word, it typically means you've gone into a place and have managed to drive everyone else out," Purpura said. "That's not the case in this instance."
Instead, it's the last provider standing. "It's more about which provider can stick it out, which one endures," Purpura said. "I know it's not as sexy as it would be to call it a 'monopoly,' but that's the actual reality."
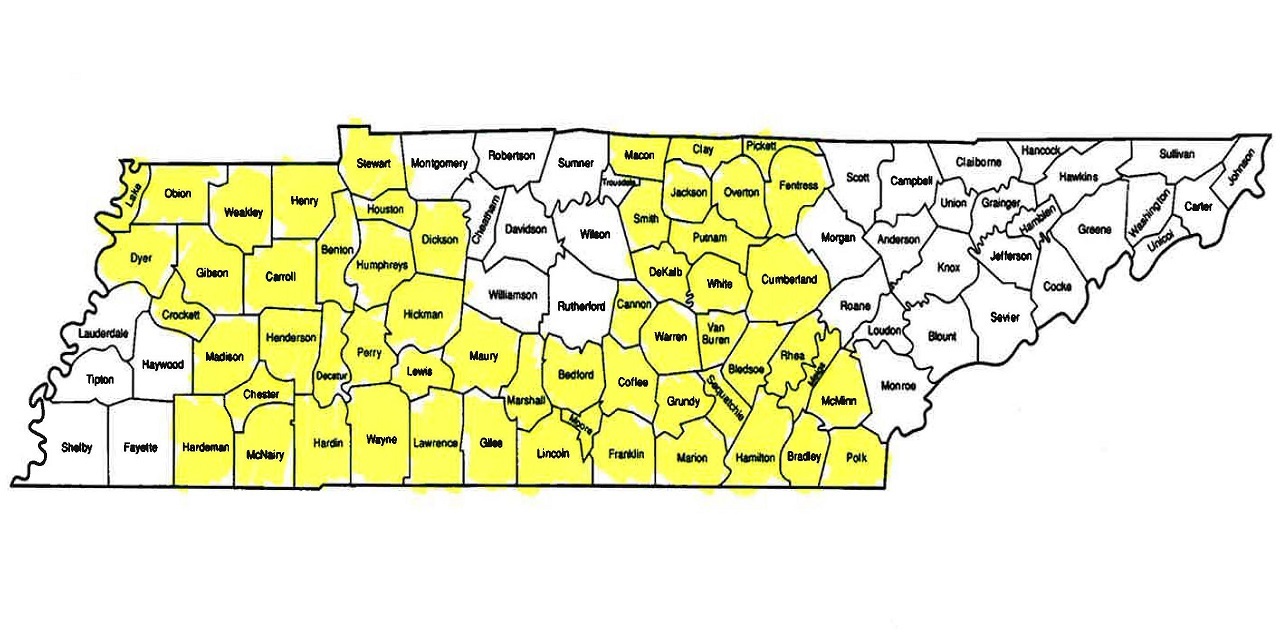
Only one provider, the nonprofit Blue Cross Blue Shield, is expected to remain standing in well more than half of Tennessee's counties in 2017 to provide health insurance coverage under the Affordable Care Act, commonly referred to as Obamacare. Based on current coverage expectations, 57 of Tennessee's 95 counties will have only one provider offering individual health care coverage under the state's exchange, based on information provided by Kevin Walters, spokesman for the Tennessee Department of Commerce and Insurance.
The commissioner for that department, Julie Mix McPeak, told The Tennessean that the situation in that the state is nearing a breaking point.
"I would characterize the exchange market in Tennessee as very near collapse," McPeak said.
Tennessee counties expected to be down to one health care insurance provider through the exchange are in the greater Chattanooga area, as well as in the western and east central part of the state.
In addition to health care insurance providers scaling back participation in Tennessee's Affordable Care Act Marketplace exchange, those who remain have announced significant premium increases. Blue Cross Blue Shield, the only health insurance provider in Tennessee that said it plans to offer coverage in all counties in the state in 2017, has said it will institute a 62 percent increase next year. Cigna plans an increase of more than 23 percent in 2017, while Humana plans an increase of 29 percent next year.
The state had to approve those increases, and that was difficult, Walters said.
"Approval of the higher rates was not an easy decision to make, nor is Tennessee alone in choosing to allow insurers to refile their requests," Walters said. "Both Illinois and Arizona have also allowed rate re-filings."
Tennessee is not the only state trying to cope with health care providers leaving Affordable Care Act exchanges and often announcing hefty increases in counties where they remain. Earlier this month, Aetna announced its plans to dramatically scale back its participation in the federally mandated health care system in 2017. Other health care insurance providers plan similar cutbacks in 2017.
In Pinal County, Arizona, no health care insurance providers are expected to offer plans under that state's Affordable Care Act Marketplace exchange in 2017. A state official there reported two health care insurance providers are willing to offer plans in that county next year, but not on the state's exchange.
Health insurance providers that have announced they are pulling out of state exchanges have cited heavy profit losses as the primary reason. Many U.S. residents -- particularly those with low incomes -- get their health care coverage from those exchanges. The Affordable Care Act mandates that most U.S. citizens acquire and maintain health insurance coverage, and those who don't face fines and other penalties. The Affordable Care Act also provides subsidies to assist lower-income people with their plans.
Tennessee's difficulties with the Affordable Care Act are the result of rising costs, Walters said.
"Tennessee has struggled to curb health care costs," Walters said. "Tennessee has some of the highest insurance-claims costs in the nation, and Tennessee has had some of the lowest rates in the nation since 2014. Cost drivers are more frequent use of health care, greater percentage with chronic diseases and rising pharmacy costs. Our actuarial consultants dug into every revised rate to determine whether the submissions were justifiable."
Even so, the state also has been trying to work with health care insurance providers in an effort to salvage the situation in Tennessee, Walters said.
"We gave insurers an opportunity to re-file their earlier rates in order to prevent total market withdrawal, which could be disastrous for consumers," Walters said. "We want Tennesseans to have coverage, but solvent insurance companies should provide that coverage."
Coverage offerings under the Affordable Care Act in Tennessee are expected to change dramatically in 2017, Walters said. Currently, no counties in the state have only one insurer on the exchange, so it will be especially jarring when 57 counties have only one provider on the exchange in 2017. Tennessee is expected to go from the 57 counties where residents currently can choose from two health care providers to 24 counties with such a choice in 2017.
While 38 Tennessee counties presently have three health care insurance providers on the exchange, only 14 counties are expected to have such a choice next year.


